Advances in the management of endometrial cancer
BMJ 2025; 388 doi: https://doi.org/10.1136/bmj-2024-080978 (Published 05 March 2025) Cite this as: BMJ 2025;388:e080978- Bradley R Corr, associate professor1,
- Britt K Erickson, associate professor2,
- Emma L Barber, assistant professor3,
- Christine M Fisher, professor4,
- Brian Slomovitz, professor5
- 1Division of Gynecologic Oncology, University of Colorado Hospital, Aurora, CO, USA
- 2Division of Gynecologic Oncology, University of Minnesota, Minneapolis, MO, USA
- 3Division of Gynecologic Oncology, Northwestern University Feinberg School of Medicine
- Chicago, IL, USA
- 4Division of Radiation Oncology, University of Colorado Hospital, Auroro, CO, USA
- 5Division of Gynecologic Oncology, Mount Sinai Medical Center, Miami, FL, USA
- Correspondence to: B R Corr Bradley.corr{at}cuanschutz.edu
ABSTRACT
Endometrial cancer is now the most lethal gynecologic malignancy, with incidence rates rising globally. Treatment strategies have historically been focused on a combination of surgery, radiation, and/or chemotherapy based primarily on histology and extent of tumor. Advances in the evaluation and treatment of endometrial cancers are occurring at a rapid pace, with a new focus on genomic profiling and targeted therapies. Surgical removal of the tumor remains the mainstay of therapy, but adjuvant treatments are a shifting paradigm. In the realm of gynecologic malignancies, endometrial cancer leads in the evolution of precision medicine. The ability to analyze patients, tumors, and therapy has increased over the past 10 years. Gaps in knowledge about racial and ethnic disparities, as well as pre-invasive disease prevention, are closing. This review describes the advances in endometrial cancer with a focus on people at risk, molecular classification, and modern therapeutic strategies.
Introduction
The lifetime risk of developing endometrial cancer is 3.1%, and the overall five year survival rate is 81%.1 The median age of diagnosis is 64; fortunately, the disease is commonly found confined to the uterus owing to the early presenting symptom of postmenopausal bleeding. When localized disease is identified and surgically removed, five year survival rates reach 95%. However, five year survival rates for distant disease are only 18%. The three major treatment modalities for endometrial cancer remain surgery, radiation, and medical therapy. The most substantial advances are in the medical treatment options for endometrial cancers. Immunotherapy has had the greatest impact on treatment recommendations, but comprehension of tumor molecular profiles and targeted treatment responses have also enabled us to treat patients with the appropriate therapies. Continued advances in all modalities of endometrial cancer treatment have ensued, with the greatest strides forward in tumor assessment and medical therapeutic agents, which are the focus of this review. In a landscape in which treatment and evaluation of endometrial cancers are continuously evolving, providers, patients, and care givers need to stay up to date. Here we review the principles of who is at risk, what tumor evaluations are available, and how these principles affect treatment modalities.
Sources and selection criteria
We obtained data from clinical trials by searching ClinicalTrials.gov for data over the past 10 years and using the terms “uterine cancer”, “endometrial cancer”, or “molecular classification”. We excluded single site clinical trials and trials that had a focus on in vitro analysis. We prioritized phase 2 and 3 clinical trials, with a focus on trials that affected global treatment strategies and novel therapeutics. We searched PubMed and Medline for review articles on endometrial cancer from 2010 to 2024 to include for analysis of trends in treatment strategies. For the molecular analysis, pre-invasive disease, and under-represented minorities sections, we searched PubMed and Medline from 2010 to January 2024 by using the molecular analysis terms associated and listed in each subgroup heading. We excluded publications not published in English as well as editorials and other non-interventional evaluations.
Epidemiology
In the US, 66 200 new cases of uterine cancer and 13 030 deaths due to the disease occurred in 2023.2 Uterine cancer is the fourth most common cancer in women (behind breast, lung, and colorectal cancer) and the sixth most deadly cancer in women. In people over 50 years old with an intact uterus, it is the second most common malignancy.3 Ovarian cancer has always been considered the most lethal gynecologic malignancy; however, in 2023 uterine cancer surpassed ovarian cancer as the most lethal gynecologic malignancy in the US.4
Despite advances in understanding of pathogenesis, risk factors, molecular subtypes, and treatment options, the incidence of endometrial cancer is increasing in the US and worldwide. More than 400 000 cases per year are estimated to occur, with the highest rates seen in North America, Europe, Micronesia/Polynesia, and Australia/New Zealand.5 Countries with the most rapid socioeconomic transitions—such as Japan, the Philippines, Belarus, Singapore, Costa Rica, and New Zealand—have seen pronounced increases in the incidence of endometrial cancer.6 Over the past two decades, the incidence has increased up to 20-fold across all age groups, and the disease is more prominent in Europe and North America than in lower income countries.56
The reasons for these national and global trends are multifactorial and not completely understood. More than 80% of endometrial cancers are estrogen receptor positive and associated with estrogen related risk factors such as obesity, nulliparity, late menopause, early menarche, and menopausal estrogen supplementation.7 Changes in fertility and reproductive factors such as fewer pregnancies and nulliparity may contribute to the rapid increase of endometrial cancer in certain countries with socioeconomic transition. Additionally, obesity is increasing worldwide and likely contributes to this trend. Other factors to consider include changes in perimenopausal hormone use, an increase in diabetes, a decrease in smoking prevalence, changes in contraceptive patterns, and changes in hysterectomy rates.6
In the US, data specific to histologic subtypes have informed our understanding of trends in endometrial cancer. When correcting for hysterectomy rates and analyzing endometrioid and non-endometrioid subtypes separately, Clarke and colleagues have shown that the dramatic rise in the incidence of endometrial cancer in the US from 2000 to 2015 is due to a sharp increase in the incidence of non-endometrioid histologic subtypes (such as serous carcinoma, clear cell carcinoma, and carcinosarcoma).8 In this same period, rates of endometrioid endometrial cancer remained consistent. Notably, the incidence of non-endometrioid endometrial cancer is highest among non-Hispanic black patients and rising most rapidly among non-Hispanic Asian/Pacific Islander patients.8
Racial and ethnic differences in endometrial cancer outcomes
Profound racial disparities exist in the incidence of endometrial cancer and death due to the disease. In the US, black people disproportionately have and die from endometrial cancer compared with white people.910 Although early reports showed that the incidence of endometrial cancer is lower in black people, differences in the prevalence of hysterectomy have likely confounded these observations. Correcting for prevalence of hysterectomy attenuates most racial disparities in incidence,11 and the overall incidence has been higher in black people since the early 2000s.39 Moreover, the number of deaths from uterine cancer have surpassed the number of deaths from ovarian cancer in black patients in the US since 2005.10 The vast majority of research on racial disparities in endometrial cancer outcomes has come from the US, with limited data resources from African, Caribbean, and European nations. However, recent data from England and Wales similarly show higher mortality rates for patients with uterine cancer from black ethnic groups compared with other ethnicities.12
Data consistently show that black patients have higher rates of recurrence of and death from endometrial cancer.13 The causes of disparities in survival are multifactorial. Black people have a disproportionate incidence of high risk histology, with non-endometrioid (including serous carcinoma and carcinosarcoma) endometrial cancer being more prevalent in black patients.3913 However, irrespective of stage or histologic subtype, black people have substantially lower five year relative survival, suggesting that disparities may be related to both biologic and non-biologic (care related) factors among black people.1415 As a single example, evaluation of microbial profiles in endometrial cancers from black and white people shows a greater microbial diversity and distinct microbial profiles in tumors from black patients.16
Tumor profiling
Molecular profiling has become more common and has allowed researchers to categorize endometrial cancer into four distinct molecular subtypes; DNA polymerase ε (POLE, ultramutated), microsatellite instability (MSI, hypermutated), copy number low, and copy number high.17 The copy number low group is often described as no specific molecular profile (NSMP), whereas the copy number high group is often delineated as TP53 on the basis of the presence of mutant p53 protein. Although rich in molecular data, tumor profiling studies are often limited in how race is defined and reported.
Stratification of a cohort of 253 molecular profiled endometrial cancer tumors by tumor histology showed no significant differences between tumors from self-reported black and white patients.18 In a separate cohort of 1882 sequentially profiled endometrial cancer tumors, somatic gene mutations did not vary between racial groups in the NSMP, microsatellite instability high (MSI-H), and POLE molecular subtypes. However, differences were seen in molecular alterations within the TP53 abnormal group. Black patients were less likely to have protein phosphatase 2 scaffold subunit Aalpha (PPP2R1A) and phosphatase and tensin homolog (PTEN) gene mutations and more frequently harbored cyclin E1 (CCNE1) amplifications, mutations in lysine methyltransferase 2B (KMT2B), breast cancer gene 1 (BRCA1), mediator complex subunit 12 (MED12), and neurofibromatosis type 1 (NF1) mutations.19 Similar findings were noted in a large cohort of more than 2000 uterine serous carcinoma tumors. Results were analyzed on the basis of predicted African ancestry from single nucleotide polymorphism analysis. Tumors from patients with predicted African ancestry had more CCNE1 amplifications, and lower phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit α (PIK3CA) and PPP2R1A alterations.20 The extent to which these genomic differences truly drive disparate outcomes is not clear.
Reasons for disparities in survival are multifactorial and complex and likely extend beyond differences in tumoral mutation. For example, disparities exist in the initial assessment and diagnosis patterns in black versus white patients. A simulated cohort study of 367 073 black and white patients showed that guidelines fail to diagnose almost half of endometrial cancers in black patients given differences in ultrasonography findings related to endometrial thickness and indication for diagnostic testing.21 Doll and colleagues indicate that endometrial thickness guidelines fail to incorporate the increased rate of uterine fibroids and non-endometrioid histologies found in black women. This may help to explain why advanced stage disease is more likely to be diagnosed in black people.22
In a cohort study of more than 270 000 patients with uterine cancer, researchers identified multiple factors associated with difference in survival between black and white people with endometrial cancer.13 They found that comorbidity score, neighborhood income, insurance status (in patients <65), histologic subtype, disease stage and treatment, and “unexplained factors” all accounted for the excess relative risk of death among black patients with endometrial cancer. Studies such as this capture risk factors at a single point in time but fail to account for a patient’s more extensive reproductive history, as well as cultural influences of racism, sexism, trauma, and intersectionality. A recent critique of disparities in endometrial cancer highlighted that a narrow definition of race as purely biologic underemphasizes the role of non-biologic (and hence modifiable) contributors to racial disparities.14
Pre-invasive disease
Endometrial intraepithelial neoplasia (EIN) is a premalignant condition of the endometrium. The term EIN is defined as hyperplasia with atypia and replaced the previous classification system of endometrial hyperplasia that classified hyperplasia into four categories: simple or complex and with and without atypia. The risk of concurrent malignancy within the uterus and progression to malignancy varied widely between these categories from 1% for simple hyperplasia to 43% for complex hyperplasia with atypia.2324 The development of endometrioid endometrial cancer is a stepwise progression from hyperplasia without atypia to hyperplasia with atypia to carcinoma. Unopposed estrogen signaling has been implicated as a driver both in the development of EIN and in the progression of EIN to endometrioid endometrial cancer.
Management
Surgery
The standard of care treatment for EIN remains hysterectomy with consideration of bilateral salpingo-oophorectomy depending on menopausal status. This recommendation remains largely based on the relatively high rate of concurrent cancer of 42.7% in women undergoing hysterectomy with a preoperative diagnosis of atypical hyperplasia found in the seminal prospective cohort study of 306 patients, GOG 167.24 However, given the rising obesity epidemic, particularly among younger people, and higher rates of delayed childbearing, fertility sparing options for this premalignant condition are of increasing interest.25 Additionally, as the population ages and has higher rates of comorbid conditions, more patients will be inoperable and need alternative non-surgical options. Finally, some patients may not consent to hysterectomy for a variety of reasons and prefer non-surgical options.
Progestins
Progestins induce cellular differentiation and are an active hormonal intervention for treatment of EIN.26 Given the relative rarity of patients who choose non-surgical management, neither the dose nor the schedule for progestin agents has been standardized in clinical management guidelines. The data on non-hormonal treatment of EIN are also sometimes difficult to interpret, as EIN and grade 1 endometrioid cancers are often included together making parsing out the specific expected response rates for patients with EIN difficult.
A retrospective population based cohort study evaluated 50 patients under the age of 45 with EIN or grade 1 endometrial cancer and found that after six months of progestin therapy, 58% had persistent disease and only 23% had full resolution of their disease at last follow-up (median 23 months).27 Notably, among women who had hysterectomy in this population, the vast majority had low risk disease (complex atypical hyperplasia or grade 1 endometrial cancer) confined to the endometrium, which indicates a potential opportunity for medical treatment without worsening of oncologic outcomes. This is consistent with data from larger populations of patients with endometrial cancer, which show the safety and efficacy of fertility sparing management of early stage, low grade endometrial cancer for some women.2829
A meta-analysis of studies of progestin therapy for patients with EIN found that 86% achieve a complete response and 16% of responders ultimately have recurrence.30 Body mass index <35 has been associated with a higher resolution rate in premenopausal patients with EIN receiving progestin therapy.31 In patients with endometrial cancer, body mass index <25, maintenance therapy, and pregnancy are all associated with improved long term oncologic outcomes.28
Non-surgical management options for EIN include treatment with progestin therapy, either with a levonorgestrel intrauterine device, oral progestins, intramuscular injections, or vaginal progestins. Megestrol acetate is the oral progestin of choice for treating EIN. Dosing is 80 mg taken twice a day; previous studies of higher dose progestins for treatment of endometrial cancer did not show benefit.32 Side effects of oral progestins include weight gain, bloating, nausea, and venous thromboembolism.
On the basis of this side effect profile and difficulties with adhering to a daily regimen of oral medications, progestin-containing intrauterine devices have emerged as the non-surgical treatment of choice for EIN. In a series of more than 300 patients with atypical hyperplasia who received progestin in the form of an intrauterine device or orally, the regression rate was higher in patients receiving the intrauterine device (95%) than in those receiving oral progestins (84%).33 A more recent prospective phase 2 study of an intrauterine device for 57 patients with endometrial cancer and atypical hyperplasia showed a response rate of 91% for atypical hyperplasia, with progression evident in 5.5% of patients.34 An overall 9.5% relapse rate after initial response was also seen. The possibility of progression, as well as relapse, mandates the careful surveillance of patients selecting conservative management. This management consists of regular endometrial biopsies, generally every three to six months for the first one to two years. Response to hormonal therapy is expected to occur within six to 12 months after initiation, so lack of response on the three month biopsy is not rare. After childbearing is complete, we recommend surgery with completion hysterectomy, with or without bilateral salpingo-oophorectomy.
Novel therapies
Given that remission rates with progestin are less than 100%, pursuit of novel therapies to improve treatment of these lesions is needed. Metformin is a potential strategy as it has anti-proliferative effects and sensitizes the endometrium to the effects of progestin. One pilot study randomized patients with EIN to metformin and megestrol acetate combined compared with megestrol acetate alone. The response rate to dual therapy was better, with a higher rate of complete response (75% v 25%) and fewer non-responders (25% v 50%); however, the results were not significant, potentially because of the small sample size of only 16 patients.35 Recent in vitro and in vivo evidence shows that the combination of metformin and a progestin has a synergistic effect, with the addition of metformin causing greater suppressive effect on endometrial cancer cells than either metformin alone or progestin alone.36 Multiple reviews suggest that metformin may play a role in improving response rates of EIN to progestin, but data are conflicting.3738
Molecular classification
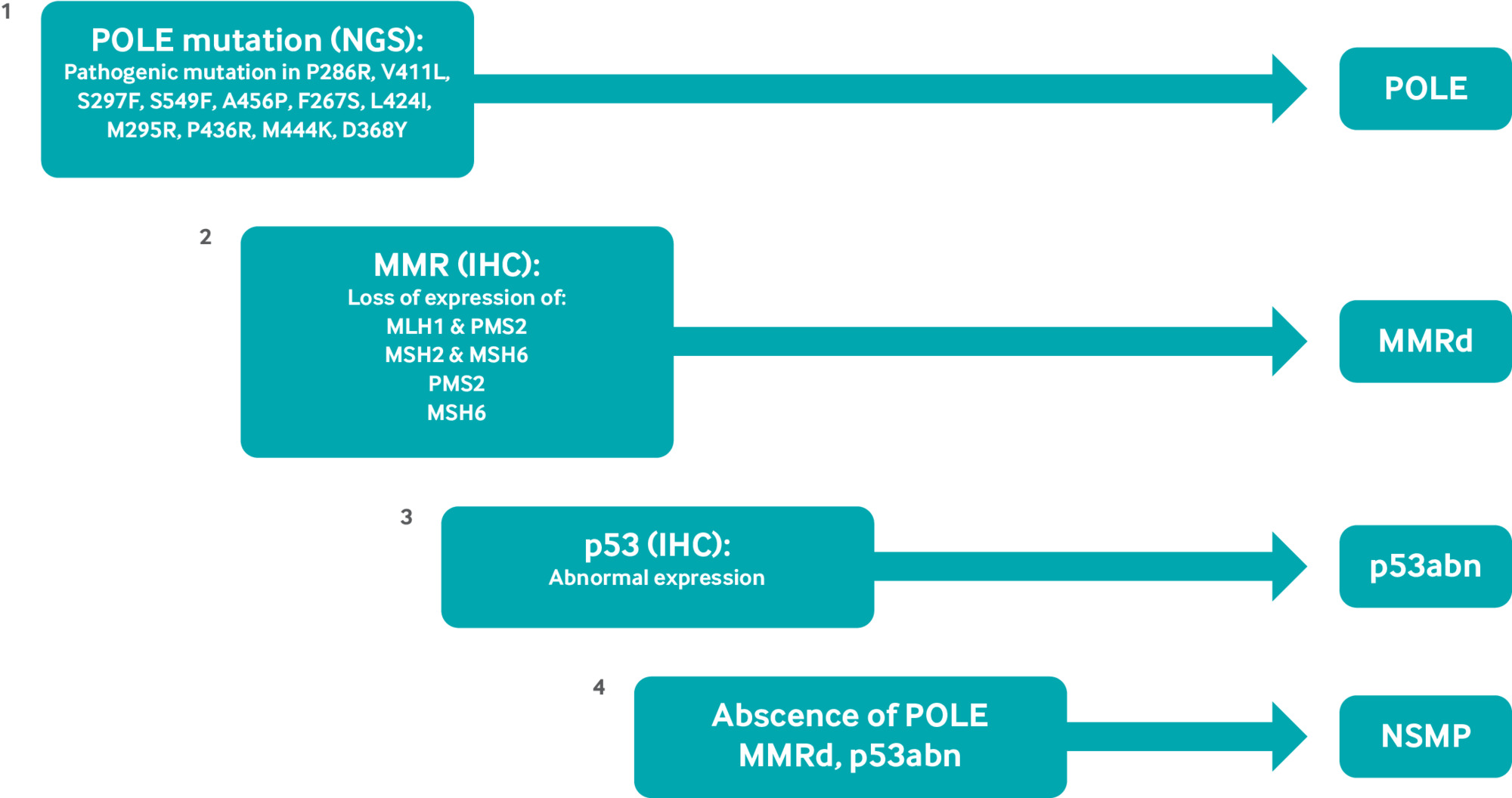
Advances in molecular analysis and the development of novel therapeutics beyond cytotoxic chemotherapies have revolutionized the characterization of and therapeutic strategies for endometrial cancer over the past decade. Whole genome sequencing was used to identify the four distinct genomic profiles initially identified by the cancer genome atlas (TCGA): POLE, MSI, copy number low, and copy number high. Subsequently, the more feasible analysis schema ProMisE (proactive molecular risk classifier for endometrial cancer) has been validated using a combination of immunohistochemistry and Sanger or next generation sequencing.173940 Each of these classifications carries with it a unique molecular profile (fig 1). However, that molecular markers exist beyond, and within, these classifications which have significant prognostic and therapeutic implications has become apparent. Human epidermal growth factor receptor 2 (HER2), estrogen receptor, progesterone receptor, catenin β 1 (CTNNB1), PTEN, phosphatidylinositol-3-kinase (PI3K)/protein kinase B (AKT)/mammalian target rapamycin (mTOR) pathway alteration, homologous recombination deficiency genes, L1 cell adhesion molecule (L1CAM), AT rich interacting domain containing protein 1A (ARID1A), and CCNE1 (cyclin E1) amplifications have all been identified as prognostic molecular markers that have been evaluated, or are being evaluated, with targeted therapeutics.41 Although each of these markers individually has shown significance in prognosis or treatment strategies, their relation within the TCGA classifications is not well defined.
TCGA/ProMise molecular classifications of endometrial cancer. DNA polymerase ε (POLE) pathogenic mutations are detected by next generation sequencing. Mismatch repair (MMR) and p53 status is determined by immunohistochemistry (IHC) staining. Evaluation is performed in order delineated. MMRd=mismatch repair deficient; NSMP=no specific molecular profile; p53abn=p53 abnormal
Historically, risk factors for recurrence of endometrial cancer were commonly described as low risk, high risk, or high intermediate risk. These classifications arose from well studied risk factors such as tumor histology, tumor grade, tumor size, depth of myometrial invasion, and presence of lymphovascular space invasion.424344 Treatment recommendations of observation, vaginal brachytherapy, whole pelvic radiation, chemotherapy, or a combination of these modalities have subsequently been evaluated in multiple phase 3 clinical trials on the basis of these well established risk factors.44454647484950
Molecular classification has progressed beyond being a solely prognostic indicator and is now an essential guide to treatment modalities in the adjuvant and recurrent disease setting. Examples include the adjuvant use of immune checkpoint blockade in stage III/IV and recurrent disease as shown by the phase 3 clinical trials RUBY/ENGOT-EN6/GOG-3031/NSGO (NCT03981796), NRG-GY018 (NCT03914612), and AtTEnd/ENGOT-en7 (NCT03603184).515253 However, ongoing clinical trials evaluating treatment modalities such as PORTEC-4a (NCT03469674; ISRCTN 11659025) and the RAINBO program (NCT05255653) plan to expand our treatment recommendations on the basis of molecular profiles.
Endometrial cancer treatment
Surgery
Surgical removal of the primary tumor with a total hysterectomy and bilateral salpingo-oopherectomy continues to be the mainstay of treatment for endometrial cancer. A minimally invasive approach is the recommended surgical approach for presumed early stage disease.5455 Surgical considerations such as lymph node evaluation, surgical staging, ovarian preservation, and surgery for advanced disease are recognized topics of discussion but will not be discussed further in this review.
Radiation
Adjuvant therapy
Use of radiation in endometrial cancer, including external beam radiation, vaginal and interstitial brachytherapy, and ablative radiation, has evolved on the basis of many clinical trials, including combinations with systemic therapy. High intermediate risk disease has been treated with a highly effective and safe modality, vaginal brachytherapy, on the basis of PORTEC 2.50 Molecular and clinicopathological analyses of PORTEC 1 and 2 show that outcomes vary by molecular subtype and have led to the design of and enrollment in PORTEC IVa,5657 using this information to selectively escalate and de-escalate outcomes. Specifically, participants in the POLE subset are de-escalated to no therapy, whereas those with p53 mutation, >10% L1CAM, and substantial lymphovascular space involvement are escalated to postoperative external beam to the pelvis. For patients with deeply invasive high grade disease and cervical stromal involvement, postoperative pelvic intensity modulated radiotherapy with or without vaginal brachytherapy remains the standard approach per GOG 249, which was a phase 3 trial of 601 patients comparing adjuvant pelvic radiation with vaginal brachytherapy plus chemotherapy in patients with high risk, early stage endometrial cancer.49
Combination therapies with chemotherapy have led to changes in more advanced disease. Molecular analysis of PORTEC 3 data indicates that specific subtypes benefit from different approaches.58 PORTEC 3 highlights the improvement with addition of chemotherapy in patients with the TP53 mutation, which comprised most recurrences and occurred early after treatment. Additionally, outcomes of patients with mismatch repair deficiency in PORTEC 3 show no additional benefit of adding chemotherapy to radiation. GOG 258 molecular subtypes have been presented with similarly intriguing findings.47 From the available data, specific subgroups that may benefit from radiation include those with more profound locoregional recurrence factors such as cervical stromal involvement, extensive lymphovascular space involvement, low grade disease in which chemotherapy may be less effective such as NSMP, and mismatch repair deficient (MMRd). These changes have been implemented to varying degrees in different countries, with the National Comprehensive Cancer Network (NCCN) guidelines incorporating them as new information becomes available.59 Given the new trials looking at chemotherapy with immunotherapy, including RUBY and GY018 without a standard radiation approach, integration of radiation with immunotherapy continues to be an area of study. GY020 (NCT04214067) is an ongoing phase 3 clinical trial evaluating radiation with or without pembrolizumab in early stage, high-intermediate risk endometrial cancers that may help to provide clarity on the efficacy of radiation and immunotherapy in endometrioid carcinomas.
Recurrent therapy
Locally and regionally recurrent disease both heavily involve radiation in the unirradiated pelvis, and occasionally with previous external beam radiation. Improvement in radiation planning and delivery, as well as advances in interstitial brachytherapy, mean that most of these patients can be cured.60 Image guided, volume directed brachytherapy has provided significant advances in multiple gynecologic cancers, including uterine cancer, and is now the standard of care in recurrent uterine cancer in the vaginal canal.61 Postoperative pelvic intensity modulated radiotherapy has become the standard of care for reduction of toxicity including gastrointestinal and bone marrow while maintaining effective outcomes.62
Ablative radiation also plays a role in patients with limited site distant recurrence.63 This is most commonly used in combination with systemic therapy, treating lung, liver, bone, lymph node, and other metastases in the oligopersistent or oligorecurrent setting in gynecologic cancer.64 Randomized trials have shown an improvement in overall survival for ablating the limited site disease versus best systemic therapy,65 and ongoing trials are using this modality in more targeted gynecologic patients.
Identifying a subset of patients with limited local and/or regional recurrence outside of previous external beam fields may enable cure, and these patients without distant metastases should be identified for multidisciplinary input. Local recurrence alone should be treated with radiation in this setting, and systemic therapy may not offer additional substantial benefit per an GOG/NRG prospective trial of 165 patients, which did not show a benefit of concurrent systemic therapy in primarily vaginal recurrences.66 For regional recurrences, concurrent systemic therapy is more commonly preferred.
For oligometastatic disease, stereotactic body radiation therapy is an effective and well recognized approach for limited site recurrences. NCCN guidelines on uterine cancer include this as a category 2B recommendation for one to five metastases with disease otherwise controlled, as well as an option for visceral disease such as liver metastases with systemic therapy.
Chemotherapy
Adjuvant therapy
Since the early 2000s chemotherapy has been the standard of care for women with advanced or recurrent endometrial cancer. Before the current regimen, the triplet of paclitaxel, adriamycin, and platinum based agents was the standard of care.67 In 2010 a randomized controlled trial reported that the combination of carboplatin and paclitaxel was equally as effective as the triplet regimen.48 In this randomized phase 3 trial of 1381 women, the progression-free survival was 13 months, overall survival was 20 months, and the response rate was 52%. The carboplatin and paclitaxel arm was also associated with a more favorable toxicity profile. Most notably, the addition of immunotherapy agents to adjuvant chemotherapy has changed the standard of care, as shown by recent approvals by governing bodies, and is discussed in detail in the dedicated immunotherapy section.
Recurrent therapy
In patients who progress after first line chemotherapy, no defined platinum-free interval or guidelines for when to retreat with platinum based therapy exist, as they do for ovarian cancer. First line trials have allowed retreatment after six to 12 months. This needs to be considered when prescribing second line therapy. Other options have not yielded significant outcomes and are often considered palliative. The two most active agents for treatment of recurrent disease are single agent doxorubicin and single agent paclitaxel dosed on a weekly regimen.686970 These agents have been investigated in phase 2 trials of 43 and 30 patients, respectively, and found to have activity. Subsequent therapy options include multiple chemotherapy agents. Unfortunately, none of them is overtly effective and they are often given in a solely palliative setting.
Immunotherapy
Immunotherapy has emerged as a key treatment for endometrial cancer. Patients who have MMRd or MSI-H endometrial cancers were initially shown to benefit from single agent therapy in the recurrent setting. Since this discovery, the use of immunotherapy has gained increasing indications and combinations in different treatment lines for patients with endometrial cancer (table 1).
Select clinical trials of single agent immunotherapy checkpoint blockade and combination therapy with immunotherapy checkpoint blockade
MMR deficiency or MSI-H status is a strong indicator of response to single agent checkpoint inhibition. Approximately 17-33% of patients with endometrial cancer will be categorized as MMRd or MSI-H.7172 Both pembrolizumab and dostarlimab have been studied as single agent treatment for these patients. In KEYNOTE-158, patients with non-colorectal MSI-H/MMRd solid tumors were enrolled and treated with pembrolizumab monotherapy at a dose of 200 mg intravenously every three weeks.73 A total of 233 patients across 27 tumor types were enrolled, with endometrial cancer being the most common tumor type, representing 21% of the entire cohort. The overall objective response rate was 34.3%, with a 57.1% objective response rate and a 25.7 month progression-free survival in patients with endometrial cancer. Patients with endometrial cancer also had the highest number of complete responses (n=8). Treatment related adverse events occurred in 64.8% of patients, with 14.6% experiencing a grade 3-5 adverse event. Confirmation of the response of patients with MMRd/MSI-H endometrial cancer to single agent checkpoint inhibition came in the phase 1/2 GARNET trial.74 Patients with MMRd/MSI-H endometrial cancer were treated with dostarlimab at an initial dose of 500 mg every three weeks; 104 women were enrolled, with an objective response rate of 42.3%, and 11.5% of patients experienced a grade 3 or higher treatment related adverse event.
Although single agent monotherapy is effective for patients with MMRd endometrial cancer, response rates in patients who are mismatch repair proficient (MMRp), which is much more common, are far less compelling.1775767778 As a result, combination therapy has been tested using lenvatinib, a receptor tyrosine kinase inhibitor, in combination with pembrolizumab in patients with endometrial cancer who have previously received at least one platinum based chemotherapy regimen. In the randomized phase 3 trial KEYNOTE-775, 827 patients with endometrial cancer (697 MMRp and 130 MMRd) were randomized 1:1 to receive lenvatinib and pembrolizumab or physician’s choice of chemotherapy (doxorubicin or paclitaxel).79 Median progression-free survival was better for patients receiving lenvatinib and pembrolizumab compared with chemotherapy (7.2 v 3.8 months; hazard ratio 0.56; P<0.001). Median overall survival was also better (18.3 v 11.4 months; hazard ratio 0.63; P<0.001). This trial led to combination lenvatinib and pembrolizumab as the standard of care for recurrent microsatellite stable endometrial cancer at the time, pre-dating use of immunotherapy in the adjuvant setting. Logically, this combination was further evaluated as first line therapy in the ENGOT-en9/LEAP-001 phase 3 trial of 842 patients (NCT03884101).80 Neither progression-free survival nor overall survival criteria were met for significant non-inferiority of lenvatinib plus pembrolizumab versus chemotherapy in the MMRp endometrial cancer population.
Immunotherapy as frontline therapy
The effectiveness of immunotherapy as second line therapy has led to investigations to move this treatment to frontline therapy. Given the efficacy of chemotherapy in inducing antigen presentation, priming tumor cells to become receptive to the immune attack triggered by checkpoint inhibitors in other tumor types, a similar strategy was tested in endometrial cancer.8182 NRG-018 was a phase 3 double blind, placebo controlled trial comparing carboplatin paclitaxel, and pembrolizumab with carboplatin, paclitaxel, and placebo among 816 patients with measurable disease (stage III or stage IVA) or stage IVB endometrial cancer.52 At 12 months, the progression-free survival was 74% among patients with mismatch repair deficiency receiving pembrolizumab and 38% among those receiving placebo (hazard ratio 0.30, 95% confidence interval 0.19 to 0.48). For patients with MMRp tumors, median progression-free survival was 13.1 months for patients on pembrolizumab and 8.7 months for those on placebo (hazard ratio 0.54, 0.41 to 0.71).
Similarly, the benefit of dostarlimab was confirmed in a phase 3 randomized controlled trial comparing carboplatin-paclitaxel-dostarlimab with carboplatin-paclitaxel-placebo among patients with stage III and IV endometrial cancer. Among the 494 patients enrolled, 23.9% were MMR deficient. Progression-free survival at 24 months was 61.4% for patients with MMR deficiency who received dostarlimab and 15.7% for those who received placebo. Overall survival at 24 months was also improved for all patients, with 71.3% alive in the dostarlimab group and 56.0% alive in the placebo group (hazard ratio 0.64, 0.46 to 0.87). Finally, a phase 3 randomized, placebo controlled, clinical trial compared atezolizumab versus carboplatin and paclitaxel in 549 patients.51 In the MMRd group, the progression-free survival showed improvement with atezolizumab (hazard ratio 0.36, 0.23 to 0.57; P<0.001) and the overall survival was improved with a hazard ratio of 0.41 (0.22 to 0.76). The MMRp group failed to show improvement in progression-free survival or overall survival. These studies show the benefit of checkpoint inhibition along with chemotherapy in improving progression-free survival, particularly for patients with MMRd disease.
Targeted therapy
Targeted therapies in endometrial cancer range from use of broad spectrum agents in select populations, such as hormonal therapies in estrogen receptor/progesterone receptor positive tumors, to directly targeting tumor antigens such as HER2 with monoclonal antibodies. With advances in drug development and molecular evaluation, multiple targets have been established (table 2).
Selected completed and ongoing clinical trials using targeted therapies in advanced and recurrent endometrial cancer
Hormonal therapies
Chemotherapy is the standard of care for patients with advanced and recurrent disease. However, low grade tumors, which can account for up to 50% of recurrences, are less likely to respond to chemotherapy. In advanced stage or recurrent disease, response rates to hormonal therapy can be up to 55%.83 Patients with estrogen receptor/progesterone receptor positive tumors are more likely to respond to these therapies. For patients with advanced or recurrent tumors that are estrogen receptor/progesterone receptor positive, hormonal agents can be considered as first line therapy. This is supported by both NCCN and European Society for Medical Oncology (ESMO) guidelines,8485 which recommend hormonal therapy for patients with recurrent, low grade endometrial cancer.
To date, no consensus exists on a definition for estrogen receptor positive status by immunohistochemical expression. Despite no standardized positive/negative score existing, a cut-off of ≥10% has been used in multiple tumor types. This value emerged from predictive models for response to endocrine therapy in breast cancer. Current American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guidelines endorse a 10% cut-off value for estrogen receptor based on prediction models of response to endocrine therapies.86 This was primarily established by an evaluation of 9639 patients with breast cancer, which found that patients with a value of ≥10% had better outcomes than did those with 1-9% or <1% expression.87 Multiple studies have further evaluated this cut-off in endometrial cancer with similar results.88899091 One study showed that estrogen receptor staining <10% was an independent predictor of worse prognosis in an evaluation of 648 NSMP tumors, but the authors acknowledge that further validation is warranted before this is translated into therapeutic trial evaluation.92
Progestins and aromatase inhibitors are commonly used as standard hormonal agents in the treatment of patients with low grade endometrial cancer. Response to progestin therapy is higher in progesterone receptor positive tumors with a well differentiated histology, and recurrence after progestins generally does not extend beyond the uterus. Use of progestin therapy has been further limited by the development of thromboembolic events.
The use of aromatase inhibition alone in endometrial cancer was studied in a phase 2 trial of 82 chemotherapy naive patients with the use of anastrozole, which showed a 9% response rate.93 This PARAGON trial focused on patients with hormone receptor positive recurrent endometrial cancer. The partial response rate was 7% and the clinical benefit rate was 44%.
Selective estrogen receptor modulators, such as tamoxifen, are also suggested as an effective hormonal therapy for endometrial carcinoma. Although tamoxifen is not effective as a single agent, several studies have looked at the sequential use of tamoxifen and progestins. GOG 153 and GOG 119 were phase 2 trials of 56 and 61 patients, respectively, and each showed higher activity of the alternating regimens compared with single agent. Response rates were 27% (38% for grade 1 tumors) and 33%, respectively, in all patients with no previous hormonal therapy or chemotherapy regardless of grade or histology. These response rates are promising and are potentially higher if the regimen is restricted to low grade endometrial cancer as a front line therapy, particularly in patients who have not received previous chemotherapy.9495
Alternative selective estrogen receptor degraders, such as fulvestrant, have also shown activity as a hormonal therapy for hormone receptor positive endometrial cancers. GOG 81 was a phase 2 trial evaluating fulvestrant in 31 patients with estrogen receptor positive advanced/metastatic endometrial cancer and showed a progression-free survival and overall survival of 10 and 26 months, respectively.96
The clinical efficacy of hormonal therapy needs to improve to achieve better outcomes. Several recent and exciting studies have suggested the use of combination hormonal therapy and other targeted therapies in patients with advanced/recurrent hormone receptor positive endometrioid endometrial cancer.
Pathological alterations in the PI3K/AKT/mTOR pathway, including loss of PTEN, occurs in 80-95% of endometrioid endometrial cancers.97 Monotherapy with mTOR inhibitors has limited activity. However, cross talk occurs between the PI3K/AKT/mTOR pathway and the estrogen receptor. mTOR inhibition is suspected to be likely to assist in overcoming resistance to hormonal therapy. A single arm, phase 2 trial of 32 patients showed that the mTOR inhibitor everolimus in combination with letrozole results in a high clinical benefit rate and high objective response rate in patients with recurrent endometrial cancer.98 Subsequently, GOG 3007 was a randomized phase 2 trial of 74 patients and looked at everolimus in combination with letrozole compared with the alternating regimen of medroxyprogesterone acetate-tamoxifen.99 On everolimus-letrozole, chemotherapy naive patients had a 28 month median progression-free survival, whereas patients who had received previous chemotherapy had a four month median progression-free survival. The results for everolimus/leterozole in chemotherapy naive patients compare favorably with the chemotherapy trials.
The PALEO trial was a randomized phase 2 trial of 77 patients that evaluated the efficacy of a cyclin dependent kinase 4/6 (CDK4/6) inhibitor, palbociclib, in combination with an aromatase inhibitor (letrozole) compared with letrozole alone in patients with advanced or recurrent estrogen receptor positive endometrial cancer.100 The combination treatment resulted in clinically meaningful progression-free survival of 8.3 months compared with 3.0 months with letrozole alone. Additional phase 2 trials with the use of CDK4/6 inhibitors have suggested synergy in combination with letrozole.101102
Anti-angiogenic therapy
Since platinum and taxanes became the standard of care, attempts have been made to combine this combination with agents other than immunotherapy. In a randomized phase 2 trial including 349 women (GOG 86P), adding bevacizumab to the combination did not improve survival outcomes in a clinically meaningful way.72 Conversely, the MITO group studied the addition of bevacizumab to carboplatin and paclitaxel in a randomized phase 2 trial of 108 women and did show increased activity.103 Nevertheless, the addition of bevacizumab has not become the standard of care. Most recently, a subgroup analysis of GOG 86P showed that those patients whose tumors had p53 mutations had a more favorable response to the addition of bevacizumab; however, the trial was not powered for this comparison.104
Emerging therapies
PARP inhibition
Poly (ADP-ribose) polymerase (PARP) inhibition is a targeted strategy used as maintenance therapy in ovarian, breast, and prostate cancers and is most effective in a BRCA mutated or homologous recombination deficient patient population. Several hypotheses have suggested that alternative DNA damage pathways can lead to efficacy in endometrial cancers. The first clinical trial of a single agent evaluating this strategy was the UTOLA trial that compared olaparib maintenance versus placebo in a randomized phase 2 trial of 147 patients.105 This trial showed no improvement in progression-free survival in the distinct patient population eligible for inclusion. However, a randomized, placebo controlled, phase 2 trial of 79 patients with metastatic/recurrent endometrial cancer comparing rucaparib versus placebo as maintenance therapy found a 55% reduction in the risk of disease progression or death (hazard ratio 0.45, 95% confidence interval 0.24 to 0.87; P=0.02).106 This correlates to an improvement in progression-free survival of 19.4 months (28.1 v 8.7 months).
The combination of PARP inhibition and immunotherapy was first determined to have potential benefit in the phase 2 DOMEC trial that evaluated the use of olaparib and durvalumab in 55 patients.107 The response rate was 16%, with a median progression-free survival of 3.4 months. In the frontline setting, the combination of PARP inhibitor along with chemotherapy and checkpoint inhibition was studied in the recently reported DUO-E/GOG-3041/ENGOT-EN10 study.108 A total of 718 patients with newly diagnosed advanced or recurrent endometrial cancer were randomly assigned 1:1:1 to carboplatin-paclitaxel plus durvalumab placebo followed by olaparib placebo maintenance (control arm); carboplatin-paclitaxel-durvalumab followed by maintenance durvalumab plus olaparib placebo (durvalumab arm); or carboplatin-paclitaxel-durvalumab followed by maintenance durvalumab plus olaparib (durvalumab+olaparib arm). A progression-free survival benefit compared with the control arm was observed in the durvalumab arm (10.2 v 9.6 months; hazard ratio 0.71; P=0.003) and in the durvalumab+olaparib arm (15.1 v 9.6 months; hazard ratio 0.55; P<0.001). These results provide an additional option for checkpoint inhibition in combination with chemotherapy in the frontline setting and provide the first evidence of potential further benefit of a PARP inhibitor in this setting. The combination strategy hypothesizes that an accumulation of DNA damage caused by the PARP inhibitor may complement the immune checkpoint blockade.
XPO1 inhibition
Selinexor is a novel therapeutic oral exportin 1 (XPO1) inhibitor that drives nuclear retention and functional activation of wild type tumor suppressor proteins, including p53. The phase 3 evaluation of this therapy as a maintenance strategy was conducted in 263 patients in the ENGOT-EN5/GOG-3055/SIENDO trial, which did not show significant improvement in progression-free survival in the intention-to-treat population.109 However, in a pre-specified evaluation of the TP53 wild type subgroup of 113 patients, the median progression-free survival was 28.4 months with selinexor versus 5.2 months with placebo. These promising results will be further evaluated in an ongoing phase 3 evaluation of this molecular subtype population (NCT05611931).
HER2 targeted therapies
Recognized for its role in other solid tumors such as breast and gastroesophageal cancer, HER2 has gained attention as a predictive and prognostic biomarker in endometrial cancer.110 Defining HER2 positivity in endometrial cancer is complex, as immunohistochemical staining patterns differ from those seen in breast cancer. Also, prospective clinical trial data specifically correlating response to HER2 targeted therapy to levels of HER2 expression based on differential scoring systems in endometrial cancer are not yet available—a crucial step in standardizing an endometrial cancer specific scoring system. Nevertheless, existing studies and clinical trials have used both the ASCO/CAP breast and gastric scoring systems and found that rates of HER2 positivity approaches 20-30% in uterine serous carcinoma.17111112113 HER2 is also expressed and amplified in uterine carcinosarcoma as well as in the more common endometrioid carcinoma.114115
In a phase 2 trial of 61 patients with HER2 positive advanced or recurrent uterine serous carcinoma, patients who received trastuzumab, a monoclonal antibody directed at HER2, had significantly improved progression-free and overall survival compared with patients who received carboplatin and paclitaxel chemotherapy alone.116 This small but landmark study led to an NCCN recommendation to include HER2 targeted therapy in the treatment strategy for patients with HER2 positive disease,117 as well as a large phase 3 study, currently ongoing, evaluating the addition of trastuzumab or pertuzuamb-trastuzumab to standard chemotherapy for patients with HER2 positive uterine serous or carcinosarcoma (NCT05256225).
Antibody-drug conjugates (ADCs) directed at HER2 have quickly gained traction in the treatment of recurrent HER2 positive endometrial cancer. ADCs have the benefit of more directed tumor cell kill with minimization of side effects compared with conventional chemotherapy. Additionally, newer ADCs have higher drug-to-antibody ratios, as well as high payload permeability, which may augment bystander killing effect on cells with low (or no) HER2 expression. Results from the large basket trial, DESTINY-PanTumour02, showed the efficacy of trastuzumab deruxtecan in various solid tumors.118 In the pre-defined cohort of 40 patients with HER2 expressing endometrial cancer (immunohistochemistry 2+ or 3+), the overall response rate was an impressive 57.5%, including an 84.6% response rate in the 13 patients with high HER2 expression (immunohistochemistry 3+). The STATICE trial evaluated trastuzumab deruxtecan in 32 patients with HER2 expressing carcinosarcomas (immunohistochemistry 1+, 2+, 3+).119 Response rates were similarly high with 54.5% in the HER2 high group (defined as immunohistochemistry 2+, 3+) and 70.0% in the HER2 low group (1+). Rates of grade 3+ adverse events were 61% (n=20), and these were most commonly hematologic events, although interstitial lung disease is a unique toxicity of this drug. Although larger confirmatory studies are pending, given these high response rates, this ADC is now an NCCN recommended biomarker directed therapy and has received accelerated approval by the US Food and Drug Administration for all solid tumors that have 3+ HER2 expression.84
Antibody-drug conjugates
ADCs are a novel therapeutic class used across many tumor types. In gynecologic cancers, their approvals have been limited to ovarian and cervical cancers, but significant evaluations in endometrial cancer are under way. Not all ADCs are the same. ADCs have three main components, and variation in any one has the potential to affect response. The three components are the antibody, the linker, and the payload. We commonly classify them on the basis of target antigen. The ADCs furthest advanced in evaluation and use in endometrial cancer are those targeting the HER2 antigen as discussed above. TROP2 is another target antigen with recent publication of results specific to endometrial cancer. The TROPiCS-03 study evaluated sacituzimab govitecan in a phase 2 basket study and reported on 41 patients with recurrent endometrial cancer, with an overall response rate of 22% (95% confidence interval 11% to 38%) and a clinical benefit rate of 32% (18% to 48%).120 Other agents targeting highly expressed target antigens such as folate receptor α (FRα) and B7-H4 are also under investigation (table 3).
Selected antibody-drug conjugates (ADCs) under investigation as single agent therapy in endometrial cancers
Guidelines
The impact of molecular analysis on prognosis and therapy indications has reached a point of shift into the global staging and treatment of endometrial cancers. The European Society of Gynaecological Oncology (ESGO), European Society for Radiotherapy and Oncology (ESTRO), European Society of Pathology (ESP), International Federation of Gynecology and Obstetrics (FIGO), and the NCCN have each incorporated molecular analysis into updated staging and guidelines in 2021 and 2023.84121122 In 2021 ESGO, ESTRO, and the ESP jointly produced updated management guidelines on treatment for endometrial cancer. These guidelines re-categorize the risk groups into low, intermediate, high-intermediate, and high on the basis of a combination of histopathological risk factors and molecular classifications (table 4). The molecular classification recommendation from these guidelines is to use the surrogate of the TCGA classifiers using TP53, mutS homolog 6, PMS2, and POLE. Furthermore, the guidelines encourage molecular classification of all endometrial carcinomas, especially high grade tumors. However, POLE mutational analysis may be omitted in low risk and grade 1 intermediate risk endometrial carcinoma.
In 2023 FIGO re-established its staging system to include molecular classification.121 Similar to ESGO, ESTRO, and ESP, molecular classification into the TCGA categories of POLEmut, MMRd, p53abn, and NSMP can be done by using analysis of p53, MSH6, PMS1 homolog 2, mismatch repair system component (PMS2), and POLE. Molecular classification is encouraged in all cases of endometrial carcinoma. Notable updates to the staging system are that the molecular evaluation of TP53 and POLE modify the FIGO staging in early endometrial cancers, whereas advanced stage disease staging is not modified by the molecular analysis. However, prognostic and treatment recommendations are directed by molecular classification in all tumors.
Conclusion
Endometrial cancer is now the most lethal gynecologic malignancy, with incidence levels rising year on year. However, the use of tumor molecular evaluation combined with novel targeted therapies yields promise for the treatment of all patients and families affected by this disease. Combinatory treatment strategies including surgery, radiation, and/or systemic therapies remain the mainstay of treatment pending elucidation of the stage and profile of the disease. However, the molecular profile of the tumor is becoming increasingly pertinent for both existing treatment modalities and emerging therapies. Endometrial cancer is the flagship gynecologic malignancy for precision based medicine. Novel therapeutic targets are working in parallel with advances in molecular detection. These advances and strategies are a testament to patient centered care and improving outcomes for patients with endometrial cancer.
Glossary of abbreviations
ADC—antibody-drug conjugate
AKT—protein kinase B
ASCO—American Society of Clinical Oncology
BRCA1—breast cancer gene 1
CAP—College of American Pathologists
CDK—cyclin dependent kinase
EIN—endometrial intraepithelial neoplasia
ESGO—European Society of Gynaecological Oncology
ESMO—European Society for Medical Oncology
ESP—European Society of Pathology
ESTRO—European Society for Radiotherapy and Oncology
FIGO—International Federation of Gynecology and Obstetrics
HER2—human epidermal growth factor receptor 2
L1CAM—L1 cell adhesion molecule
MMRd—mismatch repair deficient
MMRp—mismatch repair proficient
MSI-H—microsatellite instability high
mTOR—mammalian target rapamycin
NCCN—National Comprehensive Cancer Network
NSMP—no specific molecular profile
PARP—poly (ADP-ribose) polymerase
PI3K—phosphatidylinositol-3-kinase
POLE—DNA polymerase ε
PTEN—phosphatase and tensin homolog
Questions for future research
Should outcomes for future clinical trials be presented by racial/ethnic categories to ensure relatedness of under-represented minorities?
Can genomic classifications be used for determining treatment options in pre-invasive disease?
How can new molecular targets and biomarkers be incorporated into existing molecular risk stratifications?
Footnotes
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: All authors contributed to the intellectual content, literature search, preparation, editing, and critical review of the manuscript. BRC prepared the manuscript and did the final editing. BKE, ELB, CMF, and BS contributed significantly to the writing and review of the manuscript.
Funding: This work was supported in part by the University of Colorado Cancer Center’s Shared Resource funded by NCI grant P30CA046934.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: BRC has participated in advisory boards for Immunogen, Merck, AstraZeneca, GSK, Gilead, Zentalis, Corcept, and Imvax, has acted as an educational speaker for Targeted Oncology, and has received research funding from Clovis and Immunogen; BKE has participated in advisory boards for AstraZeneca, Gilead, GSK, and Merck; ELB has received grant funding from Eli Lilly and has participated in advisory boards or acted as a consultant for Merck and GSK; BS has consulted for AstraZeneca, Clovis, GSK, Genetech, Lilly, Novartis, Gilead, Seagen, Karyopharm, Addy, Circulogene, GOG Foundation, Merck, Imvax, EQRX, Nuvation, and Seagen.
Patient involvement: No patients were involved in the creation of this article.
Provenance and peer review: Commissioned; externally peer reviewed.